Hi
I know it’s been a while but I’ve had no spare creative juice to expend. So even now, this post will in-part consist of shameless self-plagiarism.
I was recently forced to give a talk on something I had no prior knowledge about, ‘MRSA: Origins and Consequences of this Superbug’ was the title. I’ll attach the slides for your pleasure. Now I actually quite like presenting, given that I know the topic. Who’d have thought that a person with a self-indulgent blog would like being the centre of attention eh? Anyways, I think that you shouldn’t bother giving a talk about something unless you can speak around the subject unprompted, and despite living through the pandemic like everyone else, I’m as close to an epidemiologist as your run of the mill Facebook mum. But fuck it, I’m some sort of scientist, surely I can figure out anything right? As it turns out, genomics is hard, and I don’t particular care for my ego being irreparably deflated for a few relatively inconsequential university credits. But what choice did I have? Let’s get into it.
Now before we talk about MRSA we have to talk about SA, staph, or his full Christian name Staphylococcus Aureus which translates to golden grapes in Greek and then Latin as apparently that’s what Alexander Ogsten thought they looked like under the microscope when discovering the bacteria in the 19th century. People in the life sciences have a habit of doing this sort of bastardised Greco Latin translation trick because they think they’re clever; in fairness, they are very clever.
Staph infections can look nasty, presenting as boils and abscesses on the skin, sometimes bloated with pus and looking like topical water balloons but about a third of people carry the bacteria asymptomatically on their skin an inside their noses. A bacterial infection calls for antibiotics. Thanks to the only happy accident Bob Ross wasn’t involved in, Alexander Fleming discovered Penicillin in 1928 and the world was saved from bacterial infections forever. Until they got clever.
The ‘MR’ part of the abbreviation stands for ‘Methicillin Resistant’, where Methicillin is a synthetic derivative of Penicillin created by the guys that gave us Lucozade and Beecham’s cold and flu tablets, a precursor company to GSK. This makes it a nightmare to treat, as the bacteria has mutated to fight against medication that’s meant to kill it which is pretty unfair if you ask me. Around a tenth of staph carriers carry a methicillin resistant strain.
For a rough timeline, the academic MRSA community like to divide the history of the condition into decades. 1960 being the decade of discovery where Prof. Patricia Jevons first observed MRSA, which was only a couple years after Methicillin was clinically introduced. There were a few outbreaks in Europe but early infection control in countries with sense like Denmark and The Netherlands contained them well enough. There was an outbreak in Mile End hospital in 1967, a few years after my dad was probably born there, but the British didn’t bother to take much notice. 1970 was the decade of complacency where there was a decrease in cases, MRSA was waiting to strike in 1980 and onwards with strains in Australia becoming resistant to other antibiotics too. This led to a decade of dawning realisation in 1990, note that realisation doesn’t mean action. Even though there was more press coverage, this didn’t manifest in good enough infection control leading to massive outbreaks in 2003-2007 in the UK.
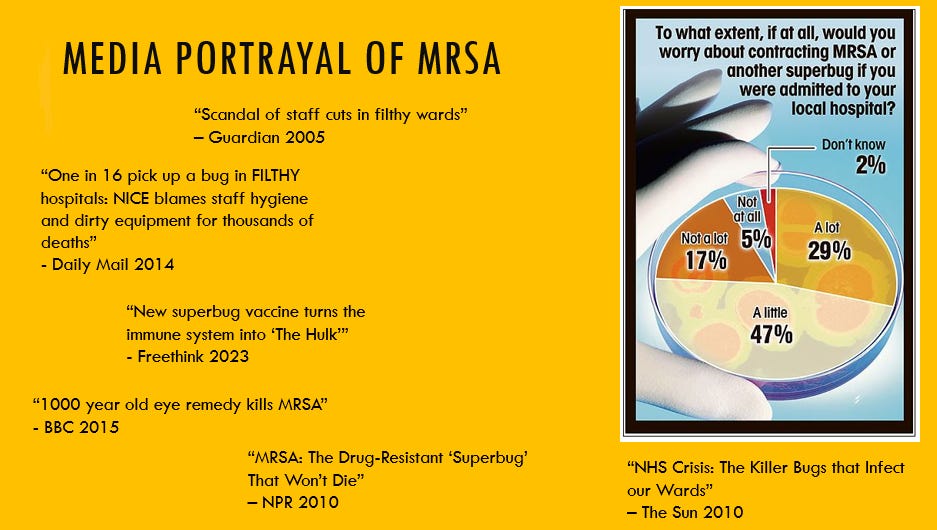
I don’t remember this as I was learning to share toys and not cry at Santa’s grotto, but apparently the media didn’t help when curbing the fear people had of going into hospital so they didn’t catch this bug. Below is an appendix slide ripped from my presentation that I had prepared for a question about public perceptions. It was never asked.
So even past the outbreak the media drove perceptions of filthy hospitals and staff that didn’t care to change that. Anyways, I’m going to pitch staph to you now, what makes it a successful pathogen. Asymptomatic Carriage and Quorum Sensing.
If anyone has ever played Plague Inc., it’s a mobile game where you make up a pathogen and try and kill everyone on the planet through adding various genetic mutations to balance the spreadability and lethality of the bug. It needs to be deadly, but not quickly enough to limit spread. It’s a balance between the lethality of Ebola and the spreadability of the common cold. An important aspect of this is being able to establish carriage in humans with no symptoms. As previously mentioned, staph does this, but as it’s spread by contact, it can be carried further without treatment. In fact, in hospitals transient carriage is a common transmission mechanism. To be a good superbug, you need to be able to spread undetected.
The next thing is a bit more sci-fi in the fact that many fantastical books and films scale up microscopic phenomena to become more scary. Quorum sensing is exactly that and it even has a cool name. It is the cell-to-cell communication where one bacterium cell releases signalling molecules that can be absorbed by others to tell them to change their gene expression, making them able to evade antibiotics and immune responses. It also facilitates the formation of biofilms, where a disgusting gooey extracellular layer encases a community of bacteria, making them harder to kill.
To make life worse, we also don’t yet have a staph vaccine due to it having the adaptability of Thomas Tuchel one nil down at half time. We’re working on it, one day we’ll get there.
There are a few risk and spread factors. An obvious one is the over prescription of antibiotics. If you kill all the bacteria that isn’t resistant to you but leave all the ones that aren’t, what do you expect to happen? Darwin award for you fella. Other factors include patient transfers and infection control measures, general close contact like playing rugby or being in prison and having medical tubing and surgical wounds. Not all avoidable but definitely manageable through being responsible with antibiotics and having up-to-standard infection control measures.
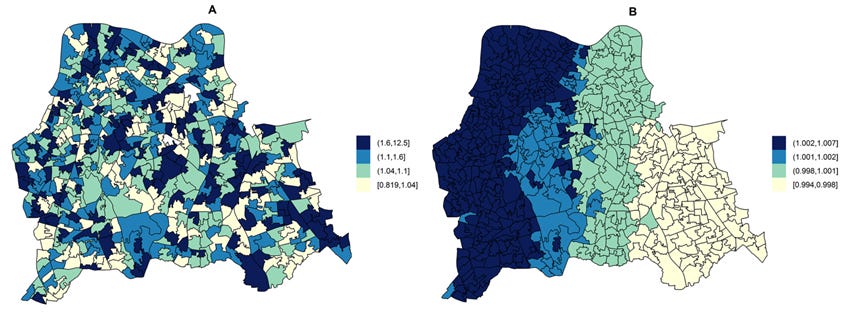
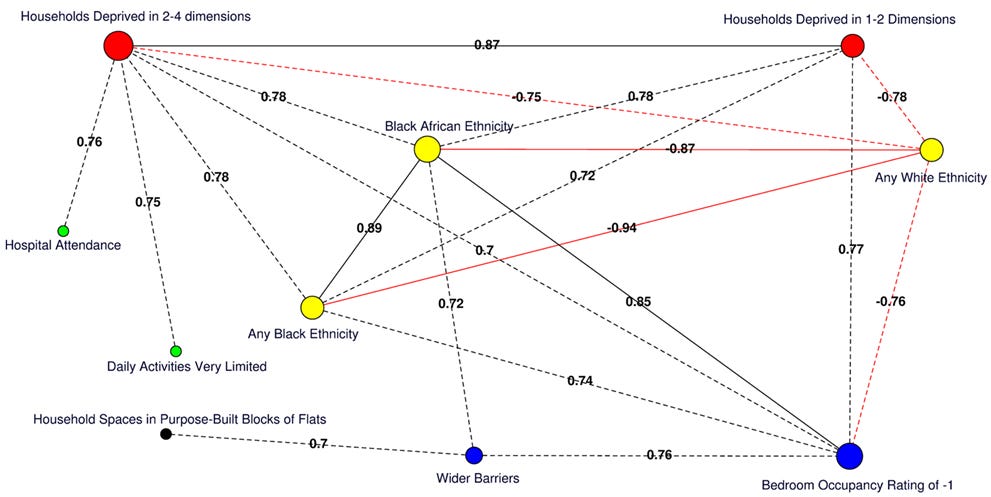
Unfortunately, once MRSA gets in the body as is untreated, it can cause some serious complications. MRSA in the blood (bacteraemia) is one of the leading serious healthcare associated infections. The two main complications arising from this are pneumonia and sepsis. Pneumonia is the inflammation of the lungs usually caused by infection and could be fatal in vulnerable groups; it accounts for nearly a fifth of global child deaths. Sepsis is the body’s serious response to infection and can lead to septic shock. It is said to be responsible for a fifth of deaths globally, around 50k a year in the UK alone. Even surviving septic shock can lead to long-term negative effects known as post-sepsis syndrome, 40% of survivors experience some form of this such as chronic fatigue or even PTSD. Note that complications from MRSA are not shared equally. In fact, this is a good opportunity to talk a bit about health inequity. It’s been shown time and time again that MRSA complications occur more in more deprived areas, key factors being access to healthcare, close proximity to others and wider barriers to housing. When analysing this we can have a look at the difference between hospital-associated (A) and community associated (B) MRSA below. This study was for central south London but there’s more significant data where larger economic inequality is present such as areas of Brazil. It’s no surprise that economic prosperity metrics increase from left to right here.
Below is the factors forming a correlation network of those in the area who contracted MRSA.
There’s also economic impact to assess but this’ll do for now cheers. email me if you want to see the whole slide deck.
References
[1] Orent, W., 2006. A brief History of Staph. Proto Magazine.
[2] Cookson, B., 2011. Five decades of MRSA: controversy and uncertainty continues. The Lancet, 378(9799), pp.1291-1292.
[3] Dutfield, G., 2009, Intellectual property rights and the life science industries: past, present and future. World Scientific. pp. 140
[4] Norfolk and Norwich University Hospitals NHS, 2022, MRSA Screening – What to expect
[5] Macal, C.M. et al., 2014. Modeling the transmission of community-associated methicillin-resistant Staphylococcus aureus, 12(1), pp.1-12.
[6] Kobayashi, S.D. and DeLeo, F.R., 2011. A MRSA-terious enemy among us: boosting MRSA vaccines. Nature medicine, 17(2), pp.168-169.
[7] Coello, R. et al., 1997. Risk factors for developing clinical infection with methicillin-resistant Staphylococcus aureus (MRSA) amongst hospital patients initially only colonized with MRSA. Journal of Hospital Infection, 37(1), pp.39-46.
[8] Safdar, N., Silva, G., Fox, B.C. and McKinley, L.M., 2016. Epidemiology of MRSA. In MRSA (pp. 24-42). CRC Press.
[9] Wang, L. and Barrett, J.F., 2007. Control and prevention of MRSA infections. Methicillin-Resistant Staphylococcus aureus (MRSA) Protocols, pp.209-225.
[10] Brent, A.J., 2021. Sepsis. Medicine, 49(11), pp.714-718.
[11] The UK Sepsis Trust, Accessed 08/11/2023, Recovery after sepsis & post sepsis syndrome
[12] Rudd, K.E. et al., 2020. Global, regional, and national sepsis incidence and mortality, 1990–2017. The Lancet, 395(10219), pp.200-211.
[13] Office for National Statistics, 2012, Deaths involving MRSA: England and Wales: 2007 to 2011
[14] Tosas, O, et al. , 2016. Evidence for Community Transmission of Community-Associated but Not Health-Care-Associated Methicillin-Resistant Staphylococcus Aureus Strains Linked to Social and Material Deprivation: Spatial Analysis of Cross-sectional Data. PLOS Medicine 13(1): e1001944.
Socials:
Instagram: mario.k.n
The website formerly known as twitter: marioknicola
Email: marioknicola@gmail.com
A song I’m listening to: